Keratoconus is a condition that affects the cornea – the clear outer layer of the eye. It causes the cornea to become thin and bulge into a cone shape instead of its usual round shape. This can lead to blurry vision and may worsen gradually over time. The resulting irregularity in the corneal curvature leads to visual distortions and impairment. Several types of keratoconus exist, each presenting unique characteristics:
Types of Keratoconus
Keratoconus, a condition affecting the cornea of the eye, can manifest in various forms. Here are the main types:
Classical Keratoconus: This is the most typical type, characterized by progressive thinning and steepening of the cornea, resulting in a cone-like shape. It’s often accompanied by visual distortions and irregular astigmatism.
Keratoglobus: Considered a rare subtype, keratoglobus affects the entire cornea, causing it to bulge outward uniformly. This results in significant visual impairment and requires specialized management.
Posterior Keratoconus: Unlike classical keratoconus, this variant primarily affects the back surface of the cornea. It leads to irregular astigmatism and may require distinct treatment approaches.
Anterior Keratoconus: In this type, the front surface of the cornea becomes steep and thin, resulting in visual blurring and distortion. It may present challenges in achieving adequate correction with glasses or contact lenses.
Keratoconus with Acute Hydrops: This is a rare complication characterized by sudden corneal swelling due to fluid buildup in the cornea. It can cause severe pain and sudden vision loss, requiring immediate medical attention.
Pellucid Marginal Degeneration: This subtype involves thinning and protrusion of the lower part of the cornea, leading to irregular astigmatism and decreased visual acuity, especially in the lower visual field.
Post-LASIK Keratectasia: Although rare, this type occurs as a complication of LASIK surgery, where the cornea becomes weak and bulges outward, causing visual disturbances similar to keratoconus.
Keratoconus in Children: While less common, keratoconus can also occur in children, posing challenges in visual development and requiring early intervention to prevent vision loss.
Understanding the different types of keratoconus is crucial for accurate diagnosis and tailored treatment plans to preserve vision and improve quality of life.
What are the Symptoms of Keratoconus?
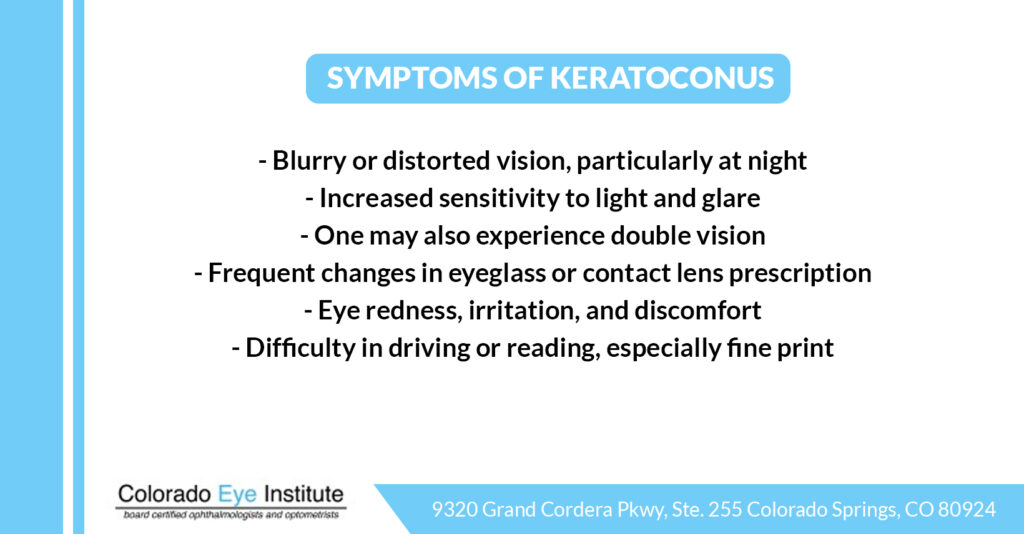
The keratoconus symptoms can be subtle initially but tend to worsen over time. They include:
- Blurry or distorted vision, particularly at night.
- Increased sensitivity to light and glare.
- One may also experience double vision.
- Frequent changes in eyeglass or contact lens prescription.
- Eye redness, irritation, and discomfort.
- Difficulty in driving or reading, especially fine print.
Stages of keratoconus
Keratoconus is a progressive eye condition characterized by the thinning and bulging of the cornea into a cone shape, leading to visual distortion and impairment. Understanding the stages of keratoconus is essential for both diagnosis and management. While the exact classification of stages may vary slightly among patients, there are generally three main stages: early, moderate, and advanced.
1. Early Stage:
In the early stage of keratoconus, the cornea begins to thin, usually in the area just below the center of the cornea. This thinning may not initially cause significant visual symptoms and can be challenging to detect without specialized tests such as corneal topography or tomography.
Patients may experience mild blurring of vision, particularly in low-light conditions or when looking at bright lights (glare).Other symptoms may include irregular astigmatism, where the cornea’s shape causes distortion of both near and distant objects, and mild sensitivity to light (photophobia). At this stage, visual correction with eyeglasses or soft contact lenses may still provide adequate vision.
2. Moderate Stage:
As keratoconus progresses into the moderate stage, the cornea continues to thin and bulge further, leading to more noticeable visual symptoms. Vision becomes significantly blurred and distorted, even with corrective lenses, as irregular astigmatism worsens.
Patients may experience increased sensitivity to light and glare, making daytime activities more challenging. Contact lens fitting becomes more complex, and rigid gas permeable (RGP) or scleral contact lenses may be required to provide better visual correction and stability. Corneal scarring may begin to develop in some cases, further impacting visual quality.
3. Advanced Stage:
In the advanced stage of keratoconus, the cornea’s thinning and protrusion become more pronounced and widespread. Vision is severely impaired, even with the most advanced contact lens options, as irregular astigmatism and distortion become extreme.
Corneal scarring may be more extensive, further reducing visual acuity and causing significant discomfort. Patients may experience significant glare, halos, and double vision, especially at night.
In some cases, the cornea may become so thin and steep that it is unable to support contact lenses, leading to difficulties in vision correction. Corneal transplantation may be considered for those with severe corneal scarring or thinning, although this is typically reserved for cases where vision cannot be adequately corrected with contact lenses.
Note: It’s essential to understand that the progression of keratoconus can vary significantly among individuals, and not all patients will experience the same stages or progression rate.
Treatment for Keratoconus
Managing keratoconus involves a range of treatment options tailored to individual needs and the stage of the condition. These may include:
Corneal Cross-Linking for Keratoconus: This innovative procedure aims to strengthen the corneal tissue using riboflavin drops and ultraviolet light exposure, potentially halting the progression of keratoconus and preserving vision.
Intacs Insertion: Intacs are small plastic rings implanted into the cornea to flatten its curvature, thereby reducing visual distortions and improving visual acuity.
Corneal Transplant: In advanced cases where other treatments are ineffective, a corneal transplant, also known as keratoplasty, may be necessary to replace the damaged corneal tissue with healthy donor tissue.
Colorado Eye Institute: Leading the Way in Keratoconus Treatment Solutions
At Colorado Eye Institute, we understand the profound impact that keratoconus can have on your vision and quality of life. That’s why we’re committed to providing comprehensive solutions of corneal cross-linking for keratoconus to meet individual needs. Located in Colorado Springs, Colorado, our facility combines advanced technology with compassionate care to deliver exceptional outcomes for patients with keratoconus. From early detection to advanced intervention, we are here to guide you through every step of your journey towards clearer vision and improved eye health.
At Colorado Eye Institute, comfort and satisfaction are our top priorities. Don’t let keratoconus hold you back from enjoying life to the fullest. Take the step towards clearer vision and better eye health by scheduling a consultation with the experts at Colorado Eye Institute. Contact us today to learn more about our innovative treatment options for keratoconus and discover how we can help you see the world more clearly.
Frequently asked questions (FAQs) about Keratoconus and Vision Impairment:
1. Can keratoconus be cured?
While there is currently no cure for keratoconus, prompt diagnosis and appropriate management can effectively control its progression and optimize visual outcomes. Cross-linking keratoconus, in particular, has shown promising results in stabilizing the condition and preserving vision.
2. Are there any risk factors associated with keratoconus?
Several factors may increase the risk of developing keratoconus, including genetic predisposition, eye rubbing habits, certain systemic conditions like Down Syndrome, and environmental triggers such as allergies and chronic eye irritation. Understanding these risk factors can aid in early detection and intervention.
3. Can keratoconus lead to blindness?
While keratoconus rarely results in complete blindness, it can cause significant visual impairment if left untreated, particularly in advanced stages. However, with timely intervention and appropriate management by getting done the procedure like Cross Linking for keratoconus, most individuals can maintain functional vision and lead fulfilling lives.
4. What happens if keratoconus is left untreated?
Untreated keratoconus can lead to the progressive deterioration of vision, increasing reliance on corrective measures, and potential complications such as corneal scarring and hydrops. Timely diagnosis and intervention are essential for preserving vision and preventing irreversible damage.
5. Can keratoconus be corrected?
While keratoconus cannot be reversed, it can be effectively managed with various treatment modalities to optimize visual acuity and quality of life. The goal of treatment is to stabilize the condition, alleviate symptoms, and restore functional vision.
6. What is the main cause of keratoconus?
The exact cause of keratoconus remains unclear, but it is believed to involve a complex interplay of genetic, environmental, and biomechanical factors. Research suggests that genetic predisposition and corneal structural abnormalities play significant roles in its development.
7. What should I not do with keratoconus?
Individuals with keratoconus should avoid rubbing their eyes vigorously, as this can exacerbate corneal thinning and increase the risk of complications. Additionally, it’s essential to adhere to prescribed treatment regimens, attend regular eye examinations, and minimize exposure to potential allergens and irritants.
8. Is keratoconus classed as a disability?
While keratoconus itself may not be classified as a disability, its impact on vision and daily functioning can vary significantly among individuals. Some individuals with advanced keratoconus may experience limitations in activities requiring clear vision, such as driving or reading small print. Depending on the severity of the condition and its impact on daily life, accommodations and support services may be available to aid affected individuals.
